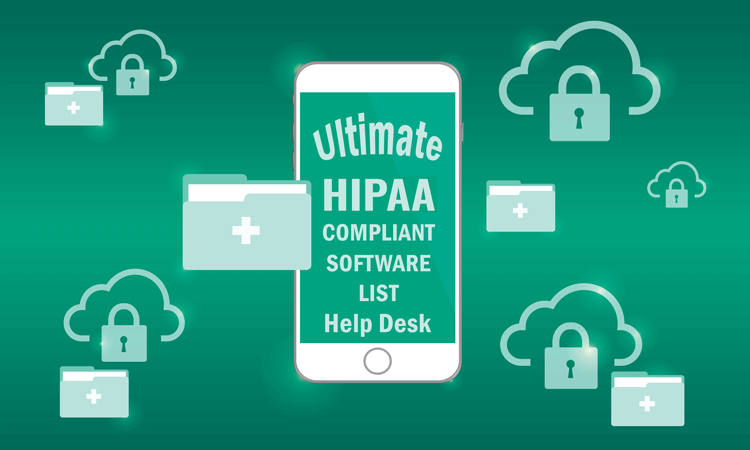
5 Top HIPAA-Compliant Apps for Therapists
With digital tools being integral to mental health care, therapists need platforms that not only streamline administrative tasks but also strictly protect client data. HIPAA-compliant apps for therapists make sure that every note, appointment, and video session is safeguarded under all required regulations and privacy standards.